Breaking down barriers to PrEP access in Aotearoa New Zealand
By Dr Rose Forster, Senior Services and Outreach Coordinator, Burnett Foundation Aotearoa
8 November 2022
Category: Clinical
Share
In response to low PrEP prescription rates in New Zealand, Burnett Foundation Aotearoa has partnered with Redseed to develop educational modules aimed at helping clinicians appropriately prescribe PrEP, and to better understand their gay and bisexual patients.
Background
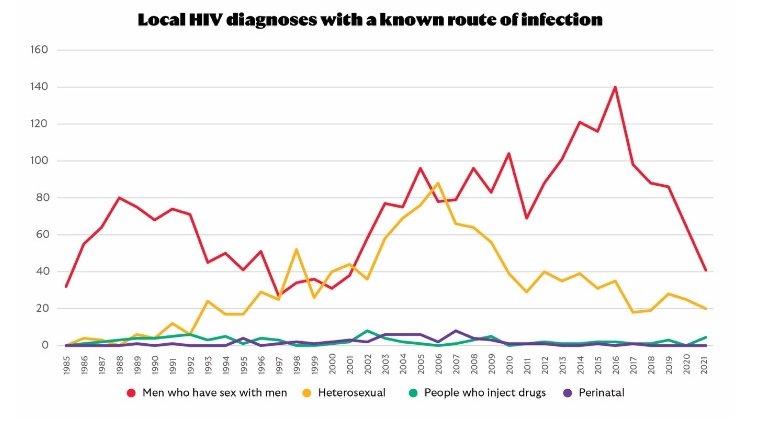
The draft National HIV Action Plan for Aotearoa New Zealand aims to eliminate HIV transmission within New Zealand by 2032. This is an achievable goal, with new notifications decreasing sharply since 2016, largely driven by a decline in new cases in men who have sex with men (MSM). Of the 112 new notifications in 2021, 67 people were first diagnosed in New Zealand, of whom 41 were MSM.
This decline in new cases is thought likely to be due to a combination of condom use, regular testing, early treatment of those who test positive, and HIV pre- and post-exposure prophylaxis (PrEP and PEP).
PrEP has been funded in New Zealand since 2018, with a widening of eligibility criteria in July 2022.
In 2021, despite 5,847 people estimated to be eligible for funded PrEP, only 1,648 (28 percent) were using it. According to Burnett Foundation Aotearoa data, around 45 percent of MSM at risk for HIV are not using any method of HIV prevention. PrEP is a significant public health initiative to prevent HIV transmission, so it’s important to understand and address barriers to access.
Survey: why people who want to use PreP, aren’t
A survey by Burnett Foundation Aotearoa showed that, of people wanting to use PrEP who weren’t currently, 48 percent did not know how to access it, 41 percent felt uncomfortable discussing PrEP with their clinician, and 15 percent could not find a GP who would prescribe PrEP. To achieve equitable access to PrEP, clinicians must actively identify patients who would benefit from PrEP, and start these conversations rather than waiting to be asked.
MSM face stigma and discrimination in life in general. Many men report negative experiences when disclosing their sexuality, and only half of our MSM population are ‘out’ to their GP. This results in missed opportunities for important health interventions. It's critical that clinicians understand how stigma impacts their patients, and are able to create an environment where patients feel comfortable discussing their sexual behaviours.
Free education modules on PrEP
Burnett Foundation Aotearoa has partnered with Redseed to develop a series of educational modules to provide the specific training that clinicians need to ensure they are appropriately prescribing PrEP and responding to the specific needs of their MSM patients.
PrEP basics
- HIV epidemiology in Aotearoa
- what PrEP is and the evidence for why it is used
- the difference between PrEP and PEP
- identifying patients who would benefit from PrEP
- special authority criteria
- medical eligibility
- conducting clinical and laboratory assessments during follow up visits
- assisting patients to cease PrEP safely.
STI management
This module links to the Aotearoa New Zealand STI Management Guidelines for use in primary care, and covers:
- the epidemiology of sexually transmitted infections (STIs) in Aotearoa
- how to screen for STIs in different population groups
- how to manage STIs, including screening, treatment, contact tracing, notification, follow-up, and prevention.
- MSM culture (module coming soon)
- unconscious bias and how it impacts on clinical interactions
- stigma and discrimination faced by MSM communities
- sexual practices and partnerships
- health challenges for MSM
- barriers to healthcare for MSM
- the role of healthcare providers in reducing these barriers, as well as sexual health recommendations for MSM.
Access these modules for free on the Burnet Foundation Aotearoa website.
