The role of radiation therapy in prostate cancer
By Dr Ben Hindson, MBChB, FRANZCR, Christchurch and Dr Doug Iupati, MBChB, FRANZCR, Wellington
7 November 2022
Category: Clinical
Share
Radiation therapy continues to be an underutilized treatment in New Zealand. The Royal Australian and New Zealand College of Radiologists (RANZCR) has reported that despite up to half of all cancer patients being considered as likely to benefit from radiation, less than a third will receive this type of treatment.2,3,4
This is also reflected in prostate cancer treatment. Brachytherapy, for example, can often be overlooked as a therapy option, due to a lack of knowledge about the treatment and its availability among healthcare professionals, despite its use in New Zealand for many years.
What is brachytherapy?
Brachytherapy involves the placement of a radiation source in or near the cancer. It’s been used by radiation oncologists for over 100 years and continues to be a commonly used treatment internationally. There is a strong history of using brachytherapy in prostate cancer, most likely related to the accessibility of the prostate gland.
Brachytherapy delivers a high radiation dose locally, with faster dose fall off peripherally. It also removes the problem of prostate movement during treatment which is a common challenge during external beam radiation therapy (EBRT). Brachytherapy can be used either alone or combined with EBRT to boost treatment dose.
In the treatment of prostate cancer, brachytherapy can be delivered one of two ways – High-Dose-Rate (HDR) or Low-Dose-Rate (LDR).
HDR involves the temporary placement of a high activity radiation source, delivering a large dose of radiation to the prostate over 10-20 minutes. It's often combined with EBRT for higher risk cancers but also as monotherapy for intermediate risk cancers.
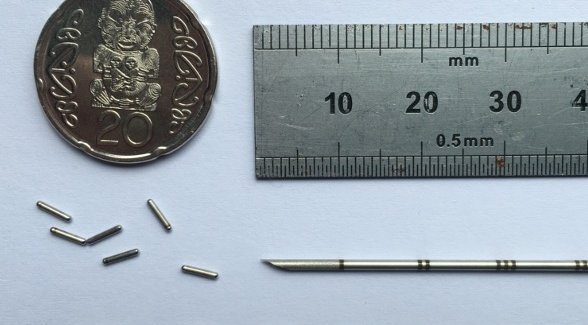
LDR brachytherapy is a well-established, minimally invasive treatment option for low or intermediate risk prostate cancer (T1-2N0M0; ISUP group 1 or 2 and PSA <20). LDR brachytherapy has been used in its modern form for over 30 years and continues to evolve. It involves permanently implanting 80-120 small radioactive Iodine1,2,5seeds, each the size of a grain of rice, into the prostate gland (Figure 1).
These have low activity (low dose rate) and emit low energy radiation that is mostly absorbed by the prostate, with very little radiation emitted externally. The seeds remain in place, emitting very low doses of radiation over a year. This approach destroys the tumor with minimum damage to the surrounding healthy tissue, and reduces disruption to ‘normal’ life.
LDR brachytherapy as a treatment option
Prostate cancer is a unique situation in which most treatment options, including surgery, EBRT and brachytherapy, offer equal cure rates.5
Each treatment option has specific impacts on the patient’s quality of life, including how long the course of treatment takes, recovery time, as well as the side effects associated with each treatment option.
LDR brachytherapy is associated with a lower risk of sexual and bladder problems and can often be performed as a day-case procedure, with most men able to return to work the following week.6,7,8
This makes it an attractive option for men living outside a major city or unable to take a lot of time off work, which can be a challenge faced with radical prostatectomy or other radiation therapy options
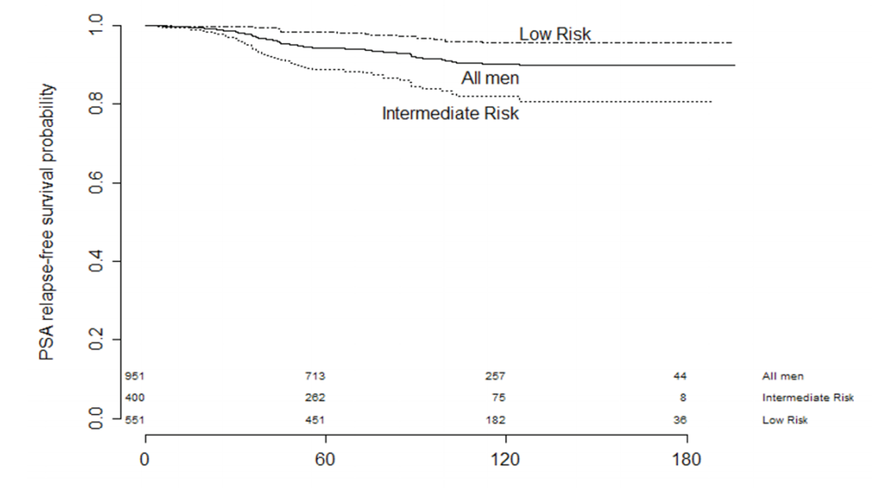
In both local and international published data on LDR brachytherapy, the 10-year PSA (prostate specific antigen) control is above 90% for all treated men.9,10 David Lamb and colleagues in Wellington have published an encouraging five-years’ worth of data demonstrating biochemical control of 95% for men with low-risk cancer and 82% for men with intermediate-risk cancer11 (Figure 2), and several series have also shown the same durable disease control in younger men (<60 years).10,12
Side effects to be considered
Erectile dysfunction (ED), urinary symptoms and bowel symptoms are side effects that need to be considered when treating prostate cancer, with ED often considered an important factor by patients. Perhaps the main advantage of LDR brachytherapy is the low risk of permanent side-effects.13
In the two months following LDR brachytherapy, men may experience temporary but significant urinary irritation and bother, however this can often be successfully managed. Late urinary bother occurs in 10% of men, urethral strictures in 2-3%, with urinary incontinence not commonly seen. Bowel toxicity is also rare, with low occurrence of significant rectal bleeding or ulceration.10,11,13,14
Evidence suggests LDR brachytherapy offers the lowest risk to erectile function compared to many other prostate cancer treatments, with Ong et al reporting 60% of men preserved excellent erectile function in the five years following treatment.15 In younger men, the erectile preservation rate was 70%.
In New Zealand, LDR brachytherapy is a combined procedure performed by both a radiation oncologist and urologist. However, the procedure also requires a multidisciplinary team including radiation therapists, medical physicists, as well as the theatre staff. The procedure is performed under general anesthetic and usually takes about an hour, with patients able to return home on the same or following day.
Unfortunately, despite the well-established use of LDR brachytherapy in New Zealand and around the world, the treatment is currently only available through New Zealand’s private health system. There is a need to improve public access to this option.
Making a treatment decision
The choice of prostate cancer treatment is a big decision for many men, and the amount of information on therapy options can be overwhelming. However, as prostate cancer is often slow growing, men and their families have an opportunity to explore all of their treatment options.
Alongside urologists and radiation oncologists, GPs play a key role in the early detection of prostate cancer through to the ongoing care of men being treated for the disease, and importantly, empowering patients and their families to make informed treatment decisions and manage side effects.
Men diagnosed with prostate cancer should be encouraged to seek multidisciplinary consultation and speak with both a urologist and radiation oncologist before making a treatment decision. We hope to see increased awareness and improved access to all treatment options for New Zealand men diagnosed with prostate cancer.
Visit the targeting cancer website for more information on radiation treatment options.
