Your Work Counts
From Monday 10 - Sunday 23 June 2024 the College’s 'Your Work Counts' project team collected data from registered members to definitively show the gap between what GPs do and what you are funded to do.
We asked members to choose any consecutive seven days (including weekends), within this two-week period, to record the time spent on five key tasks.
The five 'task types' for recording data that we asked members to use
-
Consultations
Forms of care you provide to your patients (appointments, check-ups, minor procedures etc) through any channel (phone, video, portal etc), in any setting (in practice, clinics, urgent care etc), and in any format (one-on-ones, groups, clinics etc).
View our consultations sheet for more examples.
-
Non-contact clinical time
Tasks that relate to care but aren't don't while in contact with your patients. This is a broad category which includes in-box management but also extends to liaising with other staff, interactions with the hospital system and making referrals, letters and reports.
View our non-contact clinical timesheet for more examples.
-
Training and education
The training you provide to others, the educational tasks you do for yourself, and the less formal peer and relationship activities that strengthen your networks.
View our training and education sheet for more examples.
-
Clinical governance and practice improvement
Work required to maintain patient safety and outcomes at a system level, run projects to address specific areas of community risk, and maintain relationships with the wider health sector.
View our clinical governance and practice improvement sheet for more examples.
-
Running the organisation
Things that have to be done to support the organisation from HR and employment issues, to IT and procurement, to financial management and administration.
View our running the organisation sheet for more examples.
This data will build on the results from the first diary study, which was conducted in the summer, and help us understand how winter and summer workloads compare. The data will also help the College develop evidence-based guidelines around:
- safe and sustainable patient loads
- what a fair and reasonable 40-hour week looks like
- ratios for how many GPs per 100,000 patients each region and the country needs.
Results from our first diary study
Media release: GPs working for free to complete crucial patient follow-up, study shows
“Until now, most discussions about the way we work have focused only on the patient-facing aspect. The College wants to highlight the amount of work that is actually required to look after a primary care patient load as a specialist GP or rural hospital doctor,” says College Medical Director Dr Luke Bradford.
At GP24, Dr Bradford presented the results of the second diary study (winter 2024), how they compared to the results from the summer study and outlined the next steps for the project.
“Our own terminology around work patterns has led to the impression that the only work GPs do is patient consultations, and how the current model is funded is based almost entirely on those contacts and the 15-minute consult.”
RESULTS
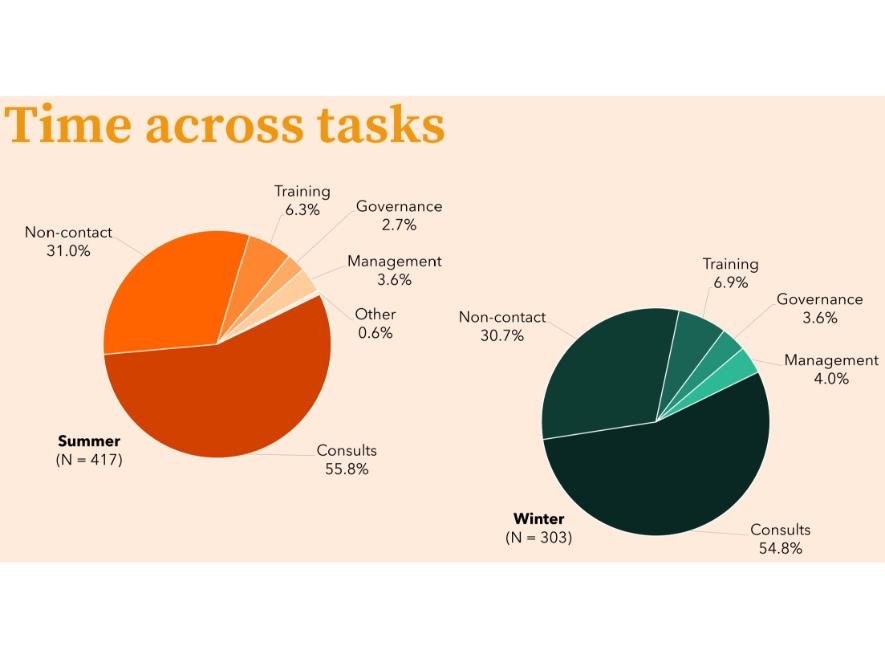
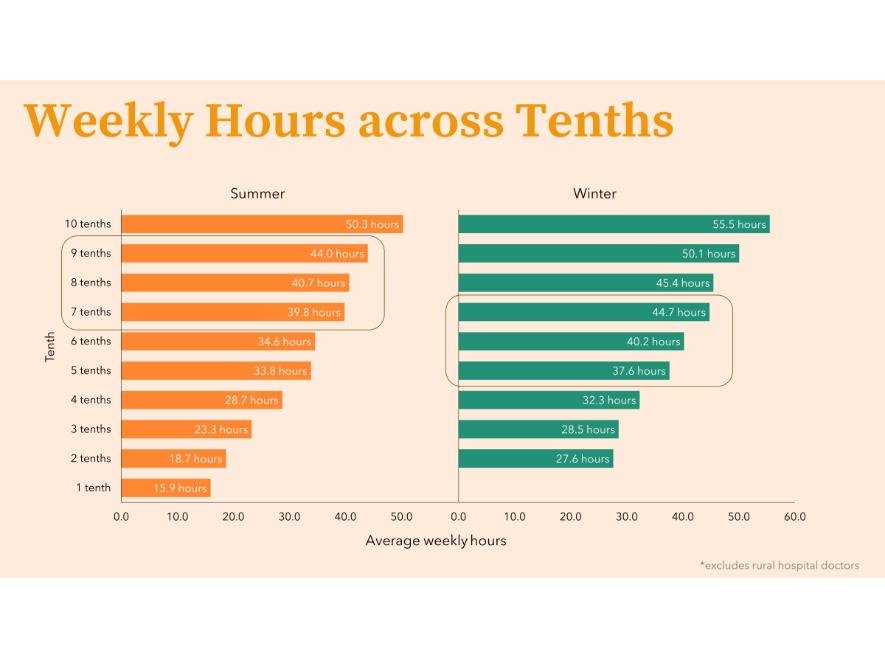
Looking at the results from both diary studies we see a lot of consistencies and now have data to show that 'part-time' doctors are working full-time hours to complete their workloads, something the workforce has known, but never quantified.
"Part-time" vs. "Full-time"
GPs work in blocks called “tenths”. One tenth equals four hours, so working 10 tenths is equal to a 40-hour week.
In many professions, a 40-hour working week is working full-time, and this doesn’t include weekends. While there are many in the workforce who, for a variety of reasons, choose to work ‘part-time’, we need to be far more aware of what part- and full-time actually means, especially when it comes to patient loads remuneration and weekend work.
Results from the two diary studies show that 71% (summer) and 73% (winter) of participants did work on the weekend and were likely not being remunerated for this time.
Averaging the time spent on the five key tasks from both diary studies, and showing what that looks like when applied to a 40-hour week, the time spent on those key tasks becomes:
Contact time (patient consultations): 22 hours
Non-contact clinical time: 12 hours
Training and education: 3 hours
Management: 2 hours
Governance: 1 hour
Dr Bradford used patient utilisation data from a case study carried out at his own practice to see how often patients were engaging with GPs (in person and online) as well as the wider practice team, combined with the outlined 40-hour clinical working week (above) and calculated a patient load of 1,023 patients per (full time) GP.
Next steps
The College will be calling on members and encouraging them to track how patients are utilising the services at their practices across the motu. By doing this we will collate more robust data that will be used support our findings and calls for action when it comes to workforce planning and capitation modelling.
The College will be sharing this information with officials across the health sector, including the Minister of Health and organisations who represent general practice and primary care so we can continue our advocacy for a sustainable, well-resourced and GP valued workforce now and into the future.
Questions
If you've got questions or would like more information, please email simon.wright@rnzcgp.org.nz
You can also watch this webinar from 15 November 2023 where questions from members were answered and we explain more about why we're doing this project.